Eating disorders
Highlights
Eating Disorders Overview
- Eating disorders typically occur in young women.
- Bulimia nervosa involves a pattern of bingeing and purging. Many people with bulimia nervosa also suffer from depression.
- Anorexia nervosa involves a pattern of self-starvation. Patients often have an accompanying anxiety disorder (such as obsessive compulsive disorder) or depression. Patients with anorexia and depression have a high risk for suicide.
Complications of Bulimia Nervosa
Many medical problems are directly associated with bulimic behavior, including:
- Tooth erosion, cavities, and gum problems
- Water retention, swelling, and abdominal bloating
- Low potassium levels
- Irregular menstrual periods
- Swallowing problems and esophagus damage
Complications of Anorexia Nervosa
Anorexia nervosa can increase the risk for serious health problems such as:
- Hormonal changes including reproductive, thyroid, stress, and growth hormones
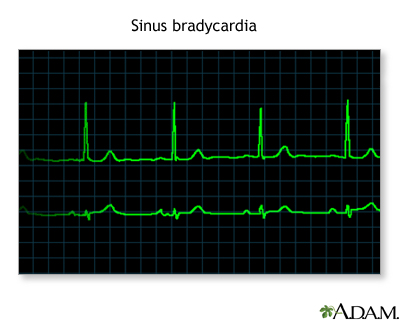
- Heart problems such as abnormal heart rhythm
- Electrolyte imbalance
- Fertility problems
- Bone density loss
- Anemia
- Neurological problems
Treatment of Bulimia Nervosa
- Bulimia nervosa is treated with a combination of psychotherapy and medication.
- Cognitive behavioral therapy, which is given along with nutritional counseling, is the preferred psychotherapeutic approach.
- Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac, generic), are the first choice for drug therapy.
Treatment of Anorexia Nervosa
- Unlike bulimia nervosa, anorexia nervosa does not respond well to drug treatment, although SSRIs are sometimes used as an adjunct to psychotherapy.
- Nutritional rehabilitation therapy, which may include the entire family, is an important part of the treatment process.
- Patients who are severely underweight and who have other physical risks may need to be hospitalized while weight is restored.
Introduction
Eating disorders are psychological problems marked by an obsession with food and weight. There are four general categories of eating disorders:
- Bulimia nervosa
- Anorexia nervosa
- Binge eating
- Eating disorders not otherwise specified
Bulimia Nervosa
Bulimia nervosa is more common than anorexia, and it usually begins early in adolescence. It is characterized by cycles of bingeing and purging, and typically takes the following pattern:
- Bulimia is often triggered when young women attempt restrictive diets, fail, and react by binge eating. Binge eating involves consuming larger than normal amounts of food within a 2-hour period.
- In response to the binges, patients compensate, usually by purging, vomiting, using enemas, or taking laxatives, diet pills, or drugs to reduce fluids.
- Patients then revert to severe dieting, excessive exercise, or both. Some patients with bulimia follow bingeing only with fasting and exercise. They are then considered to have non-purging bulimia.
- The cycle then swings back to bingeing and then to purging again.
- To be diagnosed with bulimia, a patient must binge and purge at least twice a week for 3 months.
- In some cases, the condition progresses to anorexia. Most people with bulimia, however, have a normal to high-normal body weight, although it may fluctuate by more than 10 pounds because of the binge-purge cycle.
Anorexia Nervosa
The term "anorexia" literally means absence of appetite. Anorexia can be associated with medical conditions or medications that cause a loss of appetite. Anorexia nervosa involves a psychological aversion to food that leads to a state of starvation and emaciation. In anorexia nervosa:
- At least 15% to as much as 60% of normal body weight is lost.
- The patient with anorexia nervosa has an intense fear of gaining weight, even when severely underweight.
- Individuals with anorexia nervosa have a distorted image of their own weight or shape and deny the serious health consequences of their low weight.
- Women with anorexia nervosa miss at least three consecutive menstrual periods. (Women can also be anorexic without this occurrence.)
Patients with this condition are often characterized as anorexia restrictors or anorexic bulimic. Each type is equally common.
- Anorexia restrictors reduce their weight by severe dieting.
- Anorexic bulimic patients maintain emaciation by purging. Although both types are serious, the bulimic type, which imposes additional stress on an undernourished body, is the more damaging.
Binge Eating (Binge Eating Disorder)
Bingeing without purging is characterized as compulsive overeating (binge eating) with the absence of bulimic behaviors, such as vomiting or laxative abuse (used to eliminate calories). Binge eating usually leads to becoming overweight.
To be diagnosed as a binge eater, a patient typically:
- Consumes 5,000 - 15,000 calories in one sitting
- Eats three meals a day plus frequent snacks
- Overeats continually throughout the day, rather than simply consuming large amounts of food during binges
Treatment for binge eating is usually similar to treatment for bulimia. Since binge eating is often associated with obesity, it may also require weight and dietary management. [For more information, see In-Depth Report #53: Weight control and diet.]
Eating Disorders Not Otherwise Specified
A fourth category called eating disorders not otherwise specified (EDNOS) is used to describe eating disorders not specifically defined as anorexia or bulimia. This category includes:
- Infrequent binge-purge episodes (occurring less than twice a week or having such behavior for less than months)
- Repeated chewing and spitting without swallowing large amounts of food
- Normal weight and anorexic behavior
Such patients tend to be older at diagnosis. Although less serious than other eating disorders, these patients still face similar health problems, including a higher risk for fractures.
Causes
There is no single cause for eating disorders. Although concerns about weight and body shape play a role in all eating disorders, the actual cause of these disorders appears to involve many factors, including those that are genetic and neurobiological, cultural and social, and behavioral and psychological.
Although much has been written about the roles of families and parenting as causes of eating disorders, there is no solid evidence supporting this claim.
Genetic Factors
Anorexia is eight times more common in people who have relatives with the disorder. Studies of twins show they have a tendency to share specific eating disorders (anorexia nervosa, bulimia nervosa, and obesity). Researchers have identified specific chromosomes that may be associated with bulimia and anorexia.
Biologic Factors
The body’s hypothalamic-pituitary-adrenal axis (HPA) may be important in eating disorders. This complex system originates in the following regions in the brain:
- Hypothalamus. The hypothalamus is a small structure that plays a role in controlling behaviors such as eating, sexual behavior, and sleeping, and regulates body temperature, hunger and thirst, and secretion of hormones.
- Pituitary gland. The pituitary gland is involved in controlling thyroid functions, the adrenal glands, growth, and sexual maturation.
- Amygdala. This small almond-shaped structure lies deep in the brain and is associated with regulation and control of major emotional activities including anxiety, depression, aggression, and affection.
The HPA system releases certain neurotransmitters (chemical messengers in the brain) that regulate stress, mood, and appetite. Abnormalities in the activities of three of them, serotonin, norepinephrine, and dopamine, may play a particularly important role in eating disorders. Serotonin is involved with well-being, anxiety, and appetite (among other traits), and norepinephrine is a stress hormone. Dopamine is involved in reward-seeking behavior. Imbalances with serotonin and dopamine may explain in part why people with anorexia do not experience a sense of pleasure from food and other typical comforts.
Cultural Pressures
The media plays a role in promoting unrealistic expectations for body image and a distorted cultural drive for thinness. At the same time, cheap and high-caloric foods are aggressively marketed. Such messages are contradictory and confusing.
Risk Factors
In the United States, about 7 million females and 1 million males suffer from eating disorders.
Age
Eating disorders occur most often in adolescents and young adults. However, they are becoming increasingly prevalent among young children. Eating disorders are more difficult to identify in young children because they are less commonly suspected.
Gender
Eating disorders occur predominantly among girls and women. About 90 - 95% of patients with anorexia nervosa, and about 80% of patients with bulimia nervosa, are female.
Race and Ethnicity
Most studies of individuals with eating disorders have focused on Caucasian middle-class females. However, eating disorders can affect people of all races and socioeconomic levels.
Personality Disorders
People with eating disorders tend to share similar personality and behavioral traits including low self-esteem, dependency, and problems with self-direction. Specific psychiatric personality disorders may put people at higher risk for eating disorders.
Avoidant Personality Disorder. Some studies indicate that many patients with anorexia nervosa have avoidant personalities. This personality disorder is characterized by:
- Being a perfectionist
- Being emotionally and sexually inhibited
- Wanting to be perceived as always being "good," not being rebellious
- Being terrified of being ridiculed or criticized or of feeling humiliated
People with anorexia nervosa are often extremely sensitive to failure, and any criticism, no matter how slight, may reinforce their own belief that they are "no good."
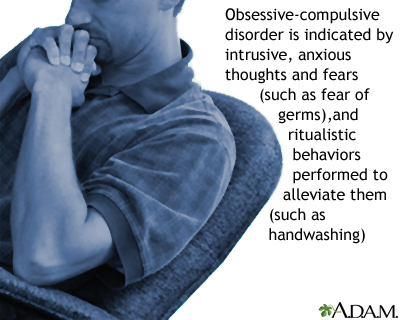
Obsessive-Compulsive Personality Disorder. Obsessive-compulsive personality disorder defines certain character traits (being a perfectionist, morally rigid, or preoccupied with rules and order). This personality disorder is strongly associated with a higher risk for anorexia. These traits should not be confused with the anxiety disorder called obsessive-compulsive disorder (OCD), although they may increase the risk for this disorder.
Borderline Personality Disorder. Borderline personality disorder (BPD) is associated with self-destructive and impulsive behaviors. People with BPD tend to have other co-existing mental health problems, including eating disorders.
Narcissistic Personality Disorder. People with narcissistic personalities tend to:
- Have an inability to soothe oneself
- Have an inability to empathize with others
- Have a need for admiration
- Be hypersensitive to criticism or defeat
Accompanying Mental Health Disorders
Many patients with eating disorders experience depression and anxiety disorders. It is not clear if these disorders, particularly obsessive-compulsive disorder (OCD), cause the eating disorders, increase susceptibility to them, or share common biologic causes.
Obsessive-Compulsive Disorder (OCD). Obsessive-compulsive disorder is an anxiety disorder that may occur in up to two thirds of patients with anorexia and up to a third of patients with bulimia. Some doctors believe that eating disorders are variants of OCD. Obsessions are recurrent or persistent mental images, thoughts, or ideas, which may result in compulsive behaviors (repetitive, rigid, and self-prescribed routines) that are intended to prevent the manifestation of the obsession. Women with anorexia and OCD may become obsessed with exercise, dieting, and food. They often develop compulsive rituals (weighing every bit of food, cutting it into tiny pieces, or putting it into tiny containers.
Other Anxiety Disorders. Other anxiety disorders associated with both bulimia and anorexia include:
- Phobias. Phobias often precede the onset of the eating disorder. Social phobias, in which a person is fearful about being humiliated in public, are common in both types of eating disorders.
- Panic Disorder. Panic disorder often follows the onset of an eating disorder. It is characterized by periodic attacks of anxiety or terror (panic attacks).
- Post-Traumatic Stress Disorder. Some patients with serious eating disorders report a past traumatic event (such as sexual, physical, or emotional abuse), and exhibit symptoms of post-traumatic stress disorder (PTSD) -- an anxiety disorder that occurs in response to life-threatening circumstances.
Depression. Depression is common in anorexia and bulimia. Major depression is unlikely to be a cause of eating disorders, however, because treating and relieving depression rarely cures an eating disorder. In addition, depression often improves after anorexic patients begin to gain weight.
Being Overweight
Extreme eating disorder behaviors, including use of diet pills, laxatives, diuretics, and vomiting, are reported more often in overweight than normal weight teenagers.
Body Image Disorders
Body Dysmorphic Disorder. Body dysmorphic disorder (BDD) involves a distorted view of one's body that is caused by social, psychologic, or possibly biologic factors. It is often associated with anorexia or bulimia, but it can also occur without any eating disorder. People with this disorder commonly suffer from emotional disorders, including obsessive-compulsive disorder and depression. As part of obsessive thinking, some people with BDD may obsess about a perceived deformity in one area of their body, and may repeatedly seek cosmetic surgery to "correct" it. People with BDD are also at higher risk for suicidal thinking and attempts.
Muscle Dysmorphia. Muscle dysmorphia is a form of body dysmorphic disorder in which the obsession involves musculature and muscle mass. It tends to occur in men who perceive themselves as being underdeveloped or "puny," which results in excessive body building, preoccupation with diet, and social problems. Such individuals are prone to eating disorders and other unhealthy behaviors, including the use of anabolic steroids.
Excessive Physical Activity
Highly competitive athletes are often perfectionists, a trait common among people with eating disorders.
Female Athletes. Excessive exercise is associated with many cases of anorexia (and, to a lesser degree, bulimia). In young female athletes, exercise and low body weight postpone puberty, allowing them to retain a muscular boyish shape without the normal accumulation of fatty tissues in breasts and hips that may blunt their competitive edge. Coaches and teachers may compound the problem by overemphasizing calorie counting and loss of body fat.
In response, people who are vulnerable to such criticism may feel compelled to strictly diet and lose weight. The term "female athlete triad" is a common and serious disorder that affects young female athletes and dancers. It includes:
- Eating disorders, including anorexia
- Amenorrhea (absent or irregular menstruation)
- Osteoporosis (bone calcium loss, which is related to low weight)
Male Athletes. Male wrestlers and lightweight rowers are also at risk for excessive dieting. Many high school wrestlers use a method called weight-cutting for rapid weight loss. This process involves food restriction and fluid depletion by using steam rooms, saunas, laxatives, and diuretics. Although male athletes are more apt to resume normal eating patterns once competition ends, studies show that the body fat levels of many wrestlers are still well below their peers during off-season and are often as low as 3% during wrestling season.
Diabetes or Other Chronic Diseases
Eating disorders may be more common in teenagers with chronic illness, such as diabetes or asthma. They are particularly serious problems for people with either type 1 or type 2 diabetes:
- Binge eating (without purging) is more common in type 2 diabetes and, in fact, the obesity it causes may even trigger this diabetes in some people.
- Both bulimia and anorexia are common among young people with type 1 diabetes. The combination of diabetes and an eating disorder can have serious health consequences. Some women with diabetes omit or underuse insulin in order to control weight. If such patients develop anorexia, their extremely low weight may appear to control the diabetes for a while. Eventually, however, if they fail to take insulin and continue to lose weight, these patients develop life-threatening complications.
Early Puberty
There appears to be a greater risk for eating disorders and other emotional problems for girls who undergo early menarche and puberty, when the pressures experienced by all adolescents are intensified by experiencing these early physical changes, including normal increased body fat.
Complications of Bulimia
Effects of Bulimic Behavior on the Body
Many medical problems are directly associated with bulimic behavior, including:
- Tooth erosion, cavities, and gum problems
- Water retention, swelling, and abdominal bloating
- Acute stomach distress
- Fluid loss with low potassium levels (due to excessive vomiting or laxative use; can lead to extreme weakness, near paralysis, or lethal heart rhythms)
- Irregular menstrual periods
- Swallowing problems and esophagus damage
Forced vomiting can cause:
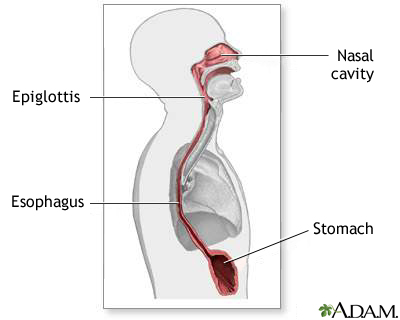
- Rupture of the esophagus
- Weakened rectal walls (rectal prolapse is a rare but serious condition that requires surgery)
Self-Destructive Behavior
A number of self-destructive behaviors occur with bulimia:
- Smoking. Many teenage girls with eating disorders smoke because they believe it will help prevent weight gain.
- Impulsive Behaviors. Women with bulimia may be at higher-than-average risk for dangerous impulsive behaviors, such as sexual promiscuity, self-cutting, and kleptomania.
- Alcohol and Substance Abuse. Many patients with bulimia abuse alcohol, drugs, or both. Women with bulimia also frequently abuse over-the-counter medications, such as laxatives, appetite suppressants, diuretics, and drugs that induce vomiting (ipecac).
Complications of Anorexia
Anorexia nervosa is a very serious illness that has a wide range of effects on the body and mind. It is frequently associated with a number of other medical problems, ranging from frequent infections and general poor health to life-threatening conditions.
Psychological Effects and Substance Abuse
Adolescents with eating behaviors associated with anorexia are at high risk for anxiety and depression in young adulthood. Patients with anorexia are at risk for suicidal behavior or attempts. Alcohol and drug abuse are also common in patients with anorexia nervosa.
Hormonal Changes
One of the most serious effects of anorexia nervosa is hormonal changes, which can have severe health consequences.
- Reproductive hormones, including estrogen and dehydroepiandrosterone (DHEA), are lowered. Estrogen is important for healthy hearts and bones. DHEA, a weak male hormone, may also be important for bone health and for other functions.
- Thyroid hormones are lower.
- Stress hormones are higher.
- Growth hormones are lower. Children and adolescents with anorexia may experience retarded growth.
The result of many of these hormonal abnormalities in women is long-term, irregular or absent menstruation (amenorrhea). This can occur early on in anorexia, even before severe weight loss. Over time this causes infertility, bone density loss, and other problems.
Heart Disease
Heart disorders are the most common medical causes of death in people with severe anorexia nervosa. The effects of anorexia on the heart include:
- Dangerous heart rhythms, including slow rhythms known as bradycardia. These abnormalities can evendevelop in teenagers with anorexia.
- Blood flow is reduced.
- Blood pressure may drop.
- The heart muscles starve, losing strength and size.
A primary danger to the heart is from imbalances of minerals, such as potassium, calcium, magnesium, and phosphate, which are normally dissolved in the body's fluid. The dehydration and starvation that occurs with anorexia can reduce fluid and mineral levels and produce a condition known as electrolyte imbalance. Certain electrolytes (especially calcium and potassium) are critical for maintaining the electric currents necessary for a normal heartbeat. An imbalance in these electrolytes can be very serious and even life threatening unless fluids and minerals are replaced. Heart problems are a particular risk when anorexia is compounded by bulimia and the use of ipecac, a drug that causes vomiting.
Effect on Fertility and Pregnancy
After treatment and an increase in weight, estrogen levels are usually restored and periods resume. In severe anorexia, however, even after treatment, normal menstruation never returns in some patients.
- If a woman with anorexia becomes pregnant before regaining normal weight, she faces a higher risk for miscarriage, cesarean section, and for having an infant with low birth weight or birth defects. She may also be at higher risk for postpartum depression.
- Women with anorexia who seek fertility treatments have lower chances for success.
Effect on Bones and Growth
Nearly all women with anorexia experience osteopenia (loss of bone calcium), and many have osteoporosis (more advanced loss of bone density). Up to two-thirds of children and adolescent girls with anorexia fail to develop strong bones during their critical growing period. Boys with anorexia also suffer from stunted growth. The less the patient weighs, the more severe the bone density loss. Women with anorexia who also binge-purge face an even higher risk for bone density loss.
Bone density loss in women is mainly due to low estrogen levels that occur with anorexia. Other biologic factors in anorexia also may contribute to bone density loss, including high levels of stress hormones (which impair bone growth) and low levels of calcium, certain growth factors, and DHEA (a weak male hormone). Weight gain, unfortunately, does not completely restore bone. Only achieving regular menstruation as soon as possible can protect against permanent bone density loss. The longer the eating disorder persists the more likely the bone density loss will be permanent.
Testosterone levels decline in boys as they lose weight, which also can affect their bone density. In young boys with anorexia, weight restoration produces some catch-up growth, but it may not produce full growth.
Neurological Problems
People with severe anorexia may suffer nerve damage that affects the brain and other parts of the body. The following nerve-related conditions have been reported:
- Seizures
- Disordered thinking
- Numbness or odd nerve sensations in the hands or feet (peripheral neuropathy)
Brain scans indicate that parts of the brain undergo structural changes and abnormal activity during anorexic states. Some of these changes return to normal after weight gain, but some damage may be permanent.
Blood Problems
Anemia (reduced number of red blood cells) is a common result of anorexia and starvation. A particularly serious blood problem is caused by severely low levels of vitamin B12. If anorexia becomes extreme, the bone marrow dramatically reduces its production of blood cells, a life-threatening condition called pancytopenia.
Gastrointestinal Problems
Bloating and constipation are both very common problems in people with anorexia.
Multiorgan Failure
In very late stages of anorexia, the organs simply fail. The main warning sign is high blood levels of liver enzymes, which require immediate administration of calories.
Complications in Adolescents with Type 1 Diabetes
Eating disorders are particularly serious for young people with type 1 diabetes.
Low blood sugar, for example, is a danger for anyone with anorexia, but it is a particularly dangerous risk for those with diabetes. If patients do not take their insulin, high blood sugar, which is also very dangerous, can occur. Unfortunately, patients with eating disorders may skip or reduce their daily insulin in order to decrease their intake of calories. Extremely high blood sugar levels can cause diabetic ketoacidosis, a condition in which acidic chemicals (ketones) accumulate in the body. This condition can lead to coma and death.
Symptoms
Symptoms Specific to Bulimia Nervosa
Symptoms or behavioral signs of bulimia may include:
- Regularly going to the bathroom right after meals
- Suddenly eating large amounts of food or buying large quantities that disappear right away
- Compulsive exercising
- Broken blood vessels in the eyes (from the strain of vomiting)
- Pouch-like appearance to the corners of the mouth due to swollen salivary glands
- Dry mouth
- Tooth cavities, diseased gums, and irreversible enamel erosion from excessive gastric acid produced by vomiting
- Rashes and pimples
- Small cuts and calluses across the tops of finger joints due to self-induced vomiting
- Evidence of discarded packaging for laxatives, diet pills, emetics (drugs that induce vomiting), or diuretics (medications that reduce fluids)
Symptoms Specific to Anorexia Nervosa
The primary symptom of anorexia is major weight loss from excessive and continuous dieting, which may either be restrictive dieting or binge-eating and purging.
Other symptoms of anorexia may include:
- Infrequent or absent menstrual periods
- Compulsive exercising coupled with excessive thinness
- Refusal to eat in front of others
- Ritualistic eating, including cutting food into small pieces
- Hypersensitivity to cold -- some women wear several layers of clothing to both keep warm and hide their thinness
- Yellowish skin, especially on the palms of the hands and soles of the feet -- from eating too many vitamin A-rich vegetables such as carrots
- Dry skin covered with fine hair
- Thin scalp hair
- Cold or swollen feet and hands
- Stomach problems, including bloating after eating
- Confused or slowed thinking
- Poor memory or judgment
Diagnosis
The first step toward a diagnosis is to admit the existence of an eating disorder. Often, the patient needs to be compelled by a parent or others to see a doctor because the patient may deny and resist the problem. Some patients may even self-diagnose their condition as an allergy to carbohydrates, because after being on a restricted diet, eating carbohydrates can produce gastrointestinal problems, dizziness, weakness, and palpitations. This may lead such people to restrict carbohydrates even more severely.
It is often extremely difficult for parents and patients to admit that a problem is present.
Screening Tests
Various questionnaires are available for assessing patients. The Eating Disorders Examination (EDE), which is an interview of the patient by the doctor, and the self-reported Eating Disorders Examination-Questionnaire (EDE-Q) are both considered valid tests for assessing eating disorder diagnosis and determining specific features of the individual’s condition (such as vomiting or laxative use).
Another test is called the SCOFF questionnaire, which can help identify patients who meet the full criteria for anorexia or bulimia nervosa. (It may not be as accurate in people who do not meet the full criteria.)
SCOFF Questionnaire
Do you make yourself Sick because you feel uncomfortably full?
Do you worry you have lost Control over how much you eat?
Have you recently lost more than One stone's worth of weight (14 pounds) in a 3-month period?
Do you believe yourself to be Fat when others say you are too thin?
Would you say that Food dominates your life?
Answering yes to two of these questions is a strong indicator of an eating disorder.
Measuring Body Mass Index
A doctor will evaluate a patient’s body mass index (BMI). The BMI is a measurement of body fat. It is derived by multiplying a person's weight in pounds by 703 and then dividing it twice by the height in inches. (BMI calculators are available online.)
- A healthy BMI for women over age 20 is 19 - 25.
- Those over 25 are considered overweight; those over 30 are considered obese.
- Those under 17.5 are considered to be at risk for health problems related to anorexia. (However, young teenagers can have lower BMIs without necessarily being anorexic.)
For example, a woman who is 5'5" and weighs 125 pounds has a healthy BMI of 21. A woman at the same height who weighs 90 pounds would have a dangerously low BMI of 15.
Diagnosing Bulimia Nervosa
A doctor generally makes a diagnosis of bulimia if there are at least two bulimic episodes per week for 3 months. Because people with bulimia tend to have complications with their teeth and gums, dentists can play a crucial role in identifying and diagnosing bulimia.
Diagnosing Anorexia Nervosa
Generally, an observation of physical symptoms and a personal history will confirm the diagnosis of anorexia. The standard criteria for diagnosing anorexia nervosa are:
- The patient's refusal to maintain a body weight normal for age and height
- Intense fear of becoming fat even though underweight
- A distorted self-image that results in diminished self-confidence
- Denial of the seriousness of emaciation and starvation
- The loss of menstrual function for at least 3 months
The doctor then categorizes the anorexia further:
- Restricting (severe dieting only)
- Anorexia bulimia (binge-purge behavior)
Diagnosing Complications of Eating Disorders
Once a diagnosis is made, a doctor will check for any serious complications of starvation and also rule out other medical disorders that might be causing the anorexia. Tests should include:
- A complete blood count
- Tests for electrolyte imbalances
- Test for protein levels
- An electrocardiogram and a chest x-ray
- Tests for liver, kidney, and thyroid problems
- A bone density test
Treatment
Treatment goals for eating disorders include:
- Restore normal weight for anorexia nervosa
- Reduce, and hopefully stop, binge eating and purging for bulimia nervosa
- Treat physical complications and any associated psychiatric disorders
- Teach patients proper nutritional habits and how to develop healthy eating patterns and meal plans
- Change patients’ dysfunctional thoughts about the eating disorder
- Improve self-control, self-esteem, and behavior
- Provide family counseling
- Prevent relapse
A multidisciplinary team approach with consistent support and counseling is essential for long-term recovery. Depending on the severity and type of eating disorder, team members may include:
- Doctors specializing in relevant medical complications
- Dietitians and nutritional counselors
- Cognitive-behavioral therapists, family therapists, or other psychotherapists
All should be experienced in treating eating disorders.
General Treatment Approaches
Eating disorders are nearly always treated with some form of psychiatric or psychologic treatment, often tied in with nutritional counseling. Depending on the disorder and the individual patient, certain psychologic approaches may work better than others.
Nutritional rehabilitation counseling is essential for recovery. It can help patients develop structured meal plans and healthy eating and weight management. In anorexia nervosa, family-based therapies that involve the parent’s assistance in feeding their adolescent child have proven to be very helpful.
Medications such as selective serotonin reuptake inhibitor (SSRI) antidepressants may be added to psychotherapy for bulimia, but there is limited evidence that these or other drugs have any significant effect on anorexia nervosa.
Although anorexia nervosa generally presents more treatment challenges than bulimia nervosa, long-term studies show recovery in many people treated for anorexia. Studies indicate that a majority of people with bulimia and up to half of patients with anorexia nervosa are free from eating disorders within 10 years of treatment.
Choosing a Treatment Setting
The patient’s condition, social circumstances, and health insurance determine the type of treatment facility -- inpatient hospitalization, residential hospitalization, partial hospitalization, or outpatient care. Patients and their families should discuss with their doctors the various options available and how structured and intense the treatment should be.
Moderately to severely ill anorexic patients may require hospitalization when:
- Weight loss continues even with outpatient treatment
- Weight is 30% below ideal body weight
- Depression is severe or the patient is suicidal
- There are symptoms of medical complications (disturbed heart rate, low potassium levels, altered mental status, low blood pressure, severe sensations of cold)
When severe metabolic or medical problems occur, patients with anorexia may need to be hospitalized either voluntarily or involuntarily. A variety of partial hospitalization or day care programs are also available.
For people with severe anorexia, many doctors recommend 10 - 12 weeks of hospitalization with full nutritional support in order for the patient to reach ideal body weight. It is particularly important for women with both diabetes and anorexia to achieve 100% of ideal weight before being released from an inpatient facility.
Treatment for Bulimia
Some doctors recommend a stepped approach for patients with bulimia, which follow specific stages depending on the severity and response to initial treatments:
- Support groups may be helpful for patients who have mild conditions with no health consequences.
- Cognitive-behavioral therapy (CBT) along with nutritional therapy is the preferred first treatment for bulimia that does not respond to support groups.
- Drug therapy used for bulimia is typically a selective serotonin-reuptake inhibitor (SSRI) antidepressant. A combination of CBT and SSRIs may be effective if CBT alone is not helpful.
Patients with bulimia rarely need hospitalization except under the following circumstances:
- Binge-purge cycles have led to anorexia
- Drugs are needed for withdrawal from purging
- Major depression is present
Psychotherapeutic Approaches and Medications for Bulimia
Psychotherapy. Cognitive-behavioral therapy (CBT) is the first-line of therapy for most patients with bulimia. Interpersonal therapy may be tried if CBT fails. In interpersonal therapy (also known as "talk therapy"), therapists help patients explore how social and family relationships may affect their eating disorder.
Antidepressants. The most common antidepressants prescribed for bulimia are selective serotonin reuptake inhibitors (SSRIs) such as:
- Fluoxetine (Prozac, generic)
- Sertraline (Zoloft, generic)
- Paroxetine (Paxil, generic)
- Fluvoxamine (Luvox, generic)
Studies are mixed, however, on whether SSRIs offer an additional advantage in reducing binge-eating compared to CBT. Fluoxetine has been approved for bulimia and is considered the drug of choice, although some studies suggest that other SSRIs work just as well. Other types of antidepressants, such as tricyclics, MAO inhibitors, and bupropion (Wellbutrin, generic), carry more risks of side effects than SSRIs and do not appear to be effective for treatment of bulimia.
Antidepressants may increase the risks for suicidal thoughts and actions during the first few months of treatment. In particular, adolescents and young adults should be carefully monitored during this time period for any changes in behavior. [For more information on antidepressants, see In-Depth Report #08: Depression.]
Other Drug Therapy for Bulimia Nervosa
Topiramate. The antiepileptic drug topiramate (Topamax, generic) has been shown in studies to reduce bingeing and purging episodes in patients with bulimia. However, due to this drug’s risk for serious side effects, topiramate should be used only if other medication has failed. In addition, because people tend to lose weight while taking topiramate, it should not be used by patients who have low or even normal body weight.
Treatment for Anorexia
Nutrition rehabilitation and psychotherapy are the cornerstones of anorexia nervosa treatment. Patients may also require treatment of medical problems related to the condition, such as bone loss, and imbalances in important electrolytes.
Restoring Normal Weight and Nutritional Intervention
Nutritional intervention is essential. Weight gain is associated with fewer symptoms of anorexia and with improvements in both physical and mental function. Restoring good nutrition can help reduce bone density loss. Raising the level of energy available to the body by balancing food intake and exercise can normalize hormonal function. Restoring weight is also essential before the patient can fully benefit from additional psychotherapeutic treatments.
Goals for Weight Gain and Good Nutrition. A weight-gain goal of 2 - 3 pounds a week for hospitalized patients, and 0.5 - 1 pound a week for outpatients, is strongly encouraged. Patients typically begin with a calorie count as low as 1,000 - 1,600 calories a day, which is then gradually increased to 2,000 - 3,500 calories a day. Patients may initially experience intensified anxiety and depressive symptoms, as well as fluid retention, in response to weight gain. These symptoms decrease as the weight is maintained.
Tubal Feedings. Feeding tubes that pass through the nose to the stomach are not commonly used, since they may discourage a return to normal eating habits and because many patients interpret their use as punishing forced feeding. However, for patients who are at significant risk or for those who refuse to eat, tube feeding through the nose or through a tube inserted through the abdomen into the stomach can help with weight gain and improve the nutritional status of the patient.
Intravenous Feedings. Intravenous feedings may be needed in life-threatening situations. This involves inserting a needle into the vein and infusing fluids containing nutrients directly into the bloodstream. Intravenous feedings must be administered carefully. When given at home, no more than the prescribed amount should be used. Overzealous administration of glucose solutions can cause phosphate levels to drop severely and trigger a condition called hypophosphatemia. Emergency symptoms include irritability, muscle weakness, bleeding from the mouth, disturbed heart rhythms, seizures, and coma.
The Maudsley Approach. For adolescent and other younger patients in the early stages of anorexia nervosa, the Maudsley approach to “refeeding” may be effective. The Maudsley approach is a type of family therapy that enlists the family as a central player in the patient’s nutritional recovery. Parents take charge of planning and supervising all of the patient’s meals and snacks. As recovery progresses, the patient gradually takes on more personal responsibility for determining when and how much to eat. Weekly family meetings and family-based counseling are also part of this therapeutic approach.
The Role of Exercise in Recovery
The role of exercise in recovery is complex, since for those with anorexia, excessive exercise is often a component of the original disorder. However, very controlled exercise regimens may be used as both a reward for developing good eating habits and as a way to reduce the stomach and intestinal distress that accompanies recovery. Exercise should not be performed if severe medical problems still exist and if the patient has not gained significant weight. The goal of exercise should be on improving physical fitness and health, not on burning off calories.
Psychologic Approaches and Medications for Patients with Anorexia Nervosa
Psychotherapy. Family therapy is an important component of anorexia treatment, especially for children and adolescents. Adults usually begin with motivational psychotherapy that provides an empathetic setting and rewards positive efforts towards weight gain. After weight is restored, cognitive behavioral therapy techniques may be helpful.
Antidepressants. Studies have not reported benefits for treating anorexia nervosa with selective serotonin reuptake inhibitors (SSRIs), the antidepressants that are often useful for patients with bulimia. A few studies suggest that these drugs could be useful for people with anorexia nervosa who also have obsessive-compulsive disorder (OCD).
Nutritional Supplements. Calcium and vitamin D supplements are often recommended. Some studies have reported that zinc supplements may help patients gain weight.
Psychotherapy
Eating disorders are nearly always treated with some form of psychotherapy. Depending on the problem, different psychological approaches may work better than others.
Cognitive-Behavioral Therapy
Cognitive-behavioral therapy (CBT) works on the principle that a pattern of false thinking and belief about one's body can be recognized objectively and altered, thereby changing the response and eliminating the unhealthy reaction to food. One approach for bulimia is the following:
- Over a period of 4 - 6 months the patient builds up to eating 3 meals a day, including foods that the patient has previously avoided.
- During this period, the patient monitors and records the daily dietary intake along with any habitual unhealthy reactions and negative thoughts toward eating while they are occurring.
- The patient also records any relapses (binges or purging). Such lapses are reported objectively and without self-criticism and judgment.
- The patient discusses the responses with a cognitive therapist at regular sessions. Eventually the patient is able to discover the false attitudes about body image and the unattainable perfectionism that underlies the opposition to food and health.
- Once these habits are recognized, food choices are broadened, and the patient begins to challenge any entrenched and automatic ideas and responses. The patient then replaces them with a set of realistic beliefs along with actions based on reasonable self-expectations.
Interpersonal Therapy
Interpersonal therapy deals with depression or anxiety that might underlie the eating disorders along with social factors that influence eating behavior. This therapy does not deal with weight, food, or body image at all.
The goals are to:
- Express feelings
- Discover how to tolerate uncertainty and change
- Develop a strong sense of individuality and independence
- Address any relevant sexual issues or traumatic or abusive event in the past that might be a contributor of the eating disorder
Studies generally report that interpersonal therapy is not as effective as cognitive therapy for bulimia and binge eating, but may be useful for some patients with anorexia. The skill of the therapist plays a strong role in its success.
Motivational Enhancement Therapy
Motivational enhancement therapy is another form of behavioral therapy that uses an empathetic approach to help patients understand and change their behaviors concerning food. It may be offered in an individual or group setting.
Family Therapy
Because a patient’s eating disorder affects the entire family, family therapy can be an important component of recovery. It can help all family members better understand the complex nature of eating disorders, improve their communication skills with one another, and teach strategies for coping with stress and negative feelings. Family-based psychotherapies are also integral parts of nutritional rehabilitation counseling programs, such as the Maudsley approach.
Resources
- www.nimh.nih.gov -- National Institute of Mental Health
- www.anad.org -- National Association of Anorexia Nervosa and Associated Disorders
- www.aedweb.org -- Academy for Eating Disorders
- www.nationaleatingdisorders.org -- Eating Disorders Awareness and Prevention
- www.eatright.org -- American Dietetic Association
- www.psych.org -- The American Psychiatric Association
- www.aacap.org -- American Academy of Child and Adolescent Psychiatry
References
American Psychiatric Association. Treatment of patients with eating disorders, third edition. American Psychiatric Association. Am J Psychiatry. 2006 Jul;163(7 Suppl):4-54.
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011 Jul;68(7):724-31.
Attia E, Walsh BT. Behavioral management for anorexia nervosa. N Engl J Med. 2009 Jan 29;360(5):500-6.
Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord. 2007 May;40(4):293-309.
Bulik CM, Berkman ND, Brownley KA, Sedway JA, Lohr KN. Anorexia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007 May;40(4):310-20.
Easter A, Treasure J, Micali N. Fertility and prenatal attitudes towards pregnancy in women with eating disorders: results from the Avon Longitudinal Study of Parents and Children. BJOG. 2011 Nov;118(12):1491-8. doi: 10.1111/j.1471-0528.2011.03077.x. Epub 2011 Aug 3.
Fisher CA, Hetrick SE, Rushford N. Family therapy for anorexia nervosa. Cochrane Database Syst Rev. 2010 Apr 14;(4):CD004780.
Golden NH, Attia E. Psychopharmacology of eating disorders in children and adolescents. Pediatr Clin North Am. 2011 Feb;58(1):121-38, xi.
Gowers SG. Management of eating disorders in children and adolescents. Arch Dis Child. 2008 Apr;93(4):331-4. Epub 2007 Oct 9.
Hall MN, Friedman RJ 2nd, Leach L. Treatment of bulimia nervosa. Am Fam Physician. 2008 Jun 1;77(11):1588, 1592.
Hunt TJ, Thienhaus O, Ellwood A. The mirror lies: body dysmorphic disorder. Am Fam Physician. 2008 Jul 15;78(2):217-22.
Ipser JC, Sander C, Stein DJ. Pharmacotherapy and psychotherapy for body dysmorphic disorder. Cochrane Database Syst Rev. 2009 Jan 21;(1):CD005332.
Kaye W. Neurobiology of anorexia and bulimia nervosa. Physiol Behav. 2008 Apr 22;94(1):121-35. Epub 2007 Nov 29.
Keel PK, Haedt A. Evidence-based psychosocial treatments for eating problems and eating disorders. J Clin Child Adolesc Psychol. 2008 Jan;37(1):39-61.
le Grange D, Lock J, Loeb K, Nicholls D. Academy for eating disorders position paper: The role of the family in eating disorders. Int J Eat Disord. 2009 Sep 2;43(1):1-5. [Epub ahead of print]
Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry. 2010 Oct;67(10):1025-32.
Ozier AD, Henry BW; American Dietetic Association. Position of the American Dietetic Association: nutrition intervention in the treatment of eating disorders. J Am Diet Assoc. 2011 Aug;111(8):1236-41.
Rosen DS; the Committee on Adolescence. Identification and management of eating disorders in children and adolescents. Pediatrics. 2010 Dec;126(6):1240-1253. Epub 2010 Nov 29.
Schmidt U, Lee S, Beecham J, et al. A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders. Am J Psychiatry. 2007 Apr;164(4):591-8.
Sim LA, McAlpine DE, Grothe KB, Himes SM, Cockerill RG, Clark MM. Identification and treatment of eating disorders in the primary care setting. Mayo Clin Proc. 2010 Aug;85(8):746-51. Epub 2010 Jul 6.
Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010 Feb 13;375(9714):583-93.
Williams PM, Goodie J, Motsinger CD. Treating eating disorders in primary care. Am Fam Physician. 2008 Jan 15;77(2):187-95.
|
Review Date:
2/8/2012 Reviewed By: David B. Merrill, MD, Assistant Clinical Professor of Psychiatry, Department of Psychiatry, Columbia University Medical Center, New York, NY. Also reviewed by Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital; and David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |




